On June 20 and 21, federal courts ruled to advance lawsuits that challenge state Medicaid exclusions of coverage for transgender health care. In Idaho, the court refused to dismiss a 14th Amendment Equal Protection case by two transgender women whose attempt to get Medicaid authorization for surgery recommended by their physicians for gender dysphoria has been repeatedly delayed, and refused to rule at this stage of the case that the state’s Medicaid medical director was immune from personal liability. In Florida, the federal court turned a preliminary injunction against the state Medicaid program exclusion of gender-affirming care into a permanent injunction after a hearing during which the plaintiffs — transgender Medicaid participants and expert witnesses for both sides — were able to present their cases.
The Idaho case, MH and TB v. Jeppesen, is pending before Chief US Magistrate Judge Raymond E. Patricco. Plaintiffs MH and TB have been receiving coverage under Medicaid for their cross-sex hormones, but their attempt to get the necessary pre-clearance for surgical care has proved exceptionally frustrating and time-consuming. MH applied for coverage for several procedures on March 10, 2021, and is still awaiting a final decision more than 13 months later.
At first, she lost on the ground that she had not completed a full year of hormone treatment, which is specified by the World Professional Association for Transgender Health treatment standards, but this turned out to be pretextual, since she had proof that she brought to an appeals hearing that she had completed the necessary year and a witness from the department conceded that the surgery would not have been approved regardless. She has filed appeals up to the level of the agency’s medical director, co-defendant Dr. Magni Hamso, but Hamso has stalled on providing a final answer.
TB sought coverage for her gender-affirming surgery in May 2022 and promptly received a “notice of decision” that stated “Outcome not rendered.” TB did not know what this meant, so she inquired several times and was advised that her request is “pending before the medical director.” It is still “pending.”
In effect, without deciding, Dr. Hamso is charged with enforcing an unwritten policy against Medicaid coverage for gender-affirming surgery. The policy became a bit less unwritten on May 1, when Governor Brad Little sent a letter to co-defendant Dave Jeppesen, director of Idaho’s Department of Health and Welfare, stating: “I oppose Idaho Medicaid using public funds to pay for irreversible sex reassignment surgeries, puberty blockers, or hormones for the purpose of changing the appearance of any child’s or adult’s sex” and “I hereby direct you and the Department of Health and Welfare to take all appropriate steps to implement a policy consistent with state and federal law excluding the same from Medicaid coverage.” Although this letter does not have the status of an official regulation, it bolsters the plaintiffs’ argument that Dr. Hamso’s stalling on authorizing their surgery constitutes a policy decision, not just a bureaucratic delay.
The state’s motion to dismiss argues that the complaint does not assert a valid equal protection claim. Judge Patricco disagrees, pointing out that Ninth Circuit precedent requires “heightened scrutiny” of state policies that discriminate against transgender people, that refusing to cover gender-affirming care is a form of discrimination since similar medical procedures are available to cisgender Medicaid participants, and that the question of whether the policy survives strict scrutiny requires fact-finding and can’t be resolved in a pretrial motion to dismiss before there is discovery and a factual record for the court to examine.
Dr. Hamso sought to avoid any personal liability by claiming qualified immunity, but Judge Patricco decided it would be inappropriate to grant her motion at this stage in the case.
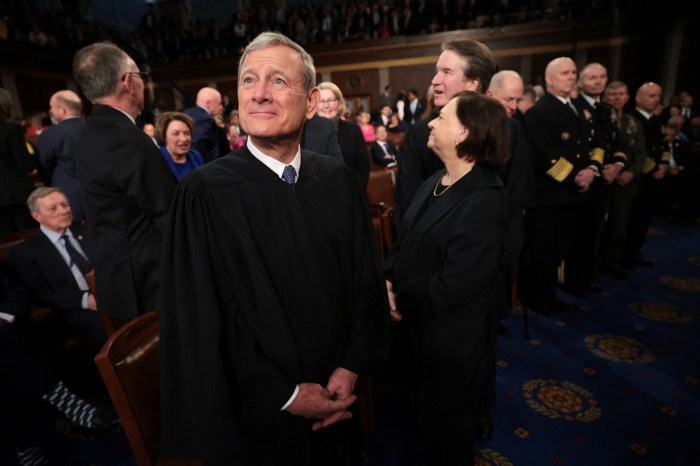
In Florida, US District Judge Robert L. Hinkle, who recently ruled that the state’s ban on gender-affirming care for minors should be preliminarily enjoined, reiterated many of the findings he made in deciding that motion to help resolve the suit by four minors who are covered by the state’s Medicaid program and are being denied coverage for gender-affirming care. In this case, Dekker v. Weida, the plaintiffs assert claims under the Equal Protection Clause, the Affordable Care Act (ACA), and the Medicaid Act. The judge was upfront about the similarity between the two cases, writing, “Many of this order’s findings and conclusions have been cut and pasted from the Doe order, with any appropriate modifications. Same record, same findings and conclusions.”
Judge Hinkle is very direct, using a bold-faced section heading to assert “Gender identity is real.” Florida’s Medicaid statute limits coverage to “medically necessary” care, and the state argues that gender-affirming care is not medically necessary. Judge Hinkle found to the contrary, and even Florida’s only credible expert witness had admitted such in the hearing testimony.
What was significant to this case was the history of how Florida Medicaid has treated the issue of gender-affirming care. When it first arose several years ago, the agency went through its usual process of evaluating new claims for service, and based on a thorough review, concluded that Medicaid should cover such services. Then, Governor Ron DeSantis, with his presidential ambitions and his “anti-woke” agenda, appointed new officials at the Health Department and the Medicaid agency who fell in line, reversing the earlier decision after holding a rigged decision process.
As Judge Hinkle described it, the new process for determining “generally accepted professional medical standards” was, “from the outset, a biased effort to justify a predetermined outcome, not a fair analysis of the evidence. The report concluded that gender-affirming medical care — puberty blockers, cross-sex hormones, and surgery — were not supported by generally accepted medical standards and were instead experimental. The conclusion was not supported by the evidence and was contrary to generally accepted medical standards.”
Based on this “flawed” report, the Florida Agency for Health Care Administration “conducted a well-choreographed public hearing that was an effort not to gather facts but to support the predetermined outcome. Afterward, AHCA adopted Florida Administrative Code rule 59G-1.050(7), barring Medicaid payment for gender-affirming puberty blockers, hormones, and surgery.” This was, of course, a political decision, not a medical decision, and thus was not entitled to the usual court deference to administrative agency expertise.
Judge Hinkle concludes that “intermediate scrutiny” applies to the equal protection claim, consistent with 11th Circuit precedent from a public employee discrimination case from several years ago. He rejects the state’s contention that it is not discriminating with respect to gender identity, but rather based on “diagnosis,” insisting that “the challenged rule and statute impose differential treatment based on sex and transgender status,” and he rejected the state’s attempt to use the Supreme Court’s Dobbs abortion ruling as justification in this case. He found the state’s justifications for its changed coverage rule to be “pretextual,” repeating (“cut and paste”) much of what he had said in his order just weeks earlier granting a preliminary injunction against the ban on gender-affirming care for minors.
The judge concluded that the plaintiffs should win their equal protection claim, their claim under the Affordable Care Act, and their claim under the Medicaid Act, pointing out that “federal law prohibits a state from denying or reducing a Medicaid-eligible patient’s required services ‘solely because of the diagnosis, type of illness, or condition.’”
“Indeed,” he continued, “denying coverage for an illness suffered only or primarily by a disfavored group is the very paradigm of prohibited discrimination based on diagnosis.” The “illness” is gender dysphoria. The “disfavored group” is transgender individuals.
“These plaintiffs are Medicaid beneficiaries who are entitled to payment, as a matter of medical necessity, for puberty blockers or cross-sex hormones as appropriately determined by their multidisciplinary teams of providers.”
However, none of the plaintiffs in the case are suing for surgery coverage, and this case is not a class action. All of the plaintiffs are concerned at this stage with continued Medicaid coverage of gender-affirming medication. One is a minor on puberty blockers who needs to continue with that and then have access to the hormones for their continued transition; a decision about surgery is years off for this plaintiff. One of the others is a young adult who was able to raise funds online to pay for surgery but needs continued access to hormones to maintain their transitional state. As a result, Judge Hinkle’s order in the case is limited to puberty blockers and hormones.
His order is a final judgment which the state can appeal to the 11th Circuit, which has a decidedly mixed record on transgender issues. The 11th Circuit was the first to have ruled in favor of a discharged transgender public employee asserting an equal protection claim. On the other hand, the circuit has become more conservative as a result of many Trump appointments, and ruled against a transgender Florida high school student challenging his school’s exclusionary restroom policy in a sharply divided en banc decision reversing the trial court. So the fate of this ruling is very much up in the air.
The plaintiffs in MH and TB, the Idaho case, are represented by Legal Aid Attorney Howard A. Belodoff. The plaintiffs in Dekker are represented by a large team of attorneys associated with Southern Legal Counsel, Florida Health Justice Project, Lambda Legal, National Health Law Program, and Pillsbury Winthrop Shaw LLP.